In Palestine, the switch to a lower-cost rotavirus vaccine paid off
Switching from one vaccine product to another can have a significant impact on a country’s budget. Health officials need to consider a variety of factors, not just vaccine price alone, to determine if making a switch makes economic sense. Sometimes this isn’t known until after the switch is completed.
The Palestinian Ministry of Health introduced the rotavirus vaccine ROTARIX® in its routine immunization program in 2016. Two years later, the Ministry decided to switch to ROTAVAC®, a rotavirus vaccine made in India. Given ROTAVAC’s lower price, such a move might seem like a clear choice. However, the overall cost of vaccination programs is influenced by a variety of vaccine characteristics, such as cold chain requirements and the number of doses required.
To evaluate the costs, impact, and cost-effectiveness of the switch from ROTARIX to ROTAVAC, PATH worked with Palestinian partners and the Rostropovich-Vishnevskaya Foundation (RVF) on an economic analysis. The results were published in PLOS ONE and summarized in a recent PATH issue brief. To learn more about the study results and their implications, we spoke with the lead study author, Frédéric Debellut.
DefeatDD: Why was an economic analysis conducted?
Fred: The study was conducted to validate the Palestinian Ministry of Health’s decision to switch rotavirus vaccines. With the additional rotavirus vaccines that became available in recent years, there is an incentive for countries to switch to products offered at lower price. But price is not the only factor affecting cost of a vaccination program. ROTARIX and ROTAVAC have different characteristics and storage requirements. Our objective was to comprehensively evaluate all the cost implications of this change. Only by accounting for all factors can we be sure of the added value brought by a new product.
DefeatDD: Why was this such a unique opportunity to conduct this analysis?
Fred: It was unique because before Palestine introduced it, ROTAVAC had not been used outside of India. And because of the established partnership between RVF and the Ministry of Health, we were able to start the study right when the switch took place.
Additionally, most studies looking at cost of delivery of rotavirus vaccines have evaluated just one single-dose vaccine. Ours was the first to compare the use of two different rotavirus vaccines in the same setting.
DefeatDD: How was the analysis conducted?
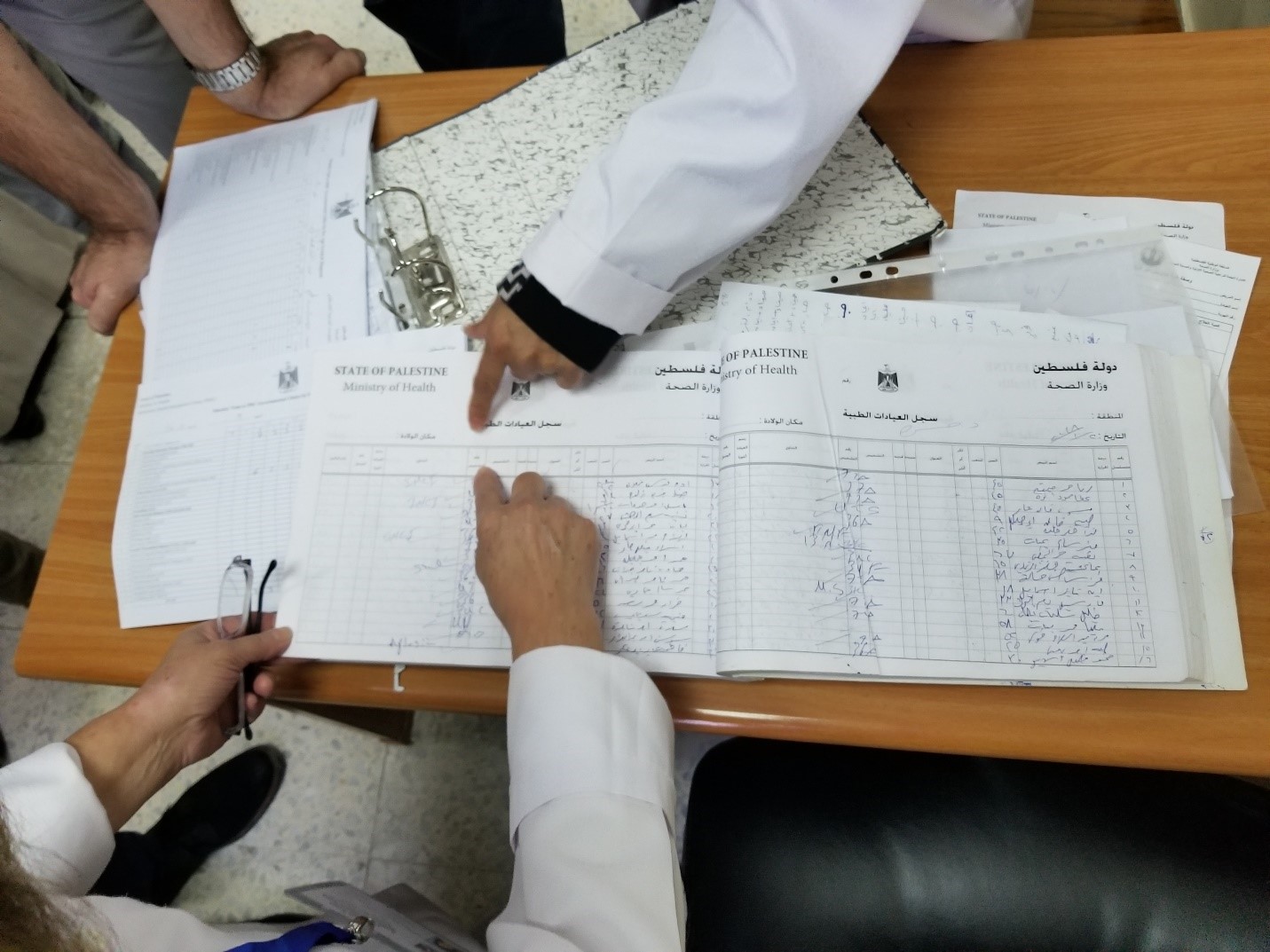
Fred: PATH worked closely with the Palestinian Ministry of Health, UN Relief and Works Agency for Palestinian Refugees in the Near East, WHO, UNICEF, and RVF to develop a study plan and methods. RVF investigators used questionnaires and visited 20 health facilities and 5 Health Directorates of Gaza and West Bank as well as the central medical store. We then plugged the data into a cost-effectiveness modeling tool called UNIVAC to generate study results. Finally, findings were disseminated in a workshop organized in Ramallah.
 The Caritas Baby Hospital in Bethlehem, West Bank, treats children with rotavirus diarrhea. Photo: PATH/Niranjan BhatDefeatDD: What are the most important takeaways from the study?
The Caritas Baby Hospital in Bethlehem, West Bank, treats children with rotavirus diarrhea. Photo: PATH/Niranjan BhatDefeatDD: What are the most important takeaways from the study?
Fred: This study provides the evidence needed to validate the government’s decision to switch to ROTAVAC. First, the study confirms that either of the rotavirus vaccines is cost-effective in Palestine. Next, we showed that it was cost-saving to change vaccines in this context. We also showed that, although the cost to deliver one dose of ROTAVAC is lower than delivering one dose of ROTARIX, the total delivery cost is less for ROTARIX as it requires only two doses. However, when coupling this with the difference in price, ROTAVAC does represent the best value for money for Palestine.
DefeatDD: Are these results useful outside of Palestine?
Fred: I think the results can be useful to other countries because they highlight the importance of assessing the different characteristics of vaccine products before deciding which vaccine to use. The study also highlights the economic benefits that can come from newly available rotavirus vaccines. For countries not yet using rotavirus vaccines, these lower-cost vaccines might provide an opportunity to introduce. For countries already using rotavirus vaccines, they may be an opportunity to create savings in their rotavirus vaccination program budget. This study may be particularly interesting for middle-income countries that finance their own immunization programs.
For more information, download the issue brief, Economic Implications of Switching Rotavirus Vaccine Products in Palestine’s Immunization Program, available in English, Arabic, French, and Russian.


