Virus variants and vaccine efficacy: 4 lessons from rotavirus
COVID-19 has highlighted the importance of studying virus diversity and the emergence of virus variants to ensure that vaccines remain effective. But in the field of virology, the potential for virus diversity to impact the effectiveness of vaccines has been the object of intense research globally for some time.
As a virologist, I focus on rotavirus, a leading cause of severe and fatal diarrheal disease in young children and a long-time subject of strain diversity research. Here are a few lessons rotavirus has taught us about virus variants and vaccines.
1. Viruses evolve. It’s what they do.
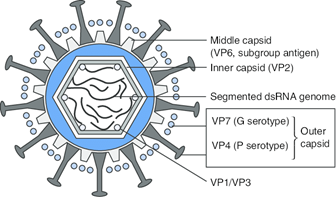 The ‘G’ and ‘P’ proteins on the outer layer (capsid) of rotavirus vary by rotavirus type. Image source. The existence and continued emergence of virus variants is normal for all viruses. Changes in the virus genome, called mutations, occur at random as they multiply. Mutations can have a big or small impact, and can affect the survival of the virus, its ability to adapt to new hosts, its transmissibility, disease severity and characteristics, and its ability to escape recognition by antibodies generated after previous infections or vaccination.
The ‘G’ and ‘P’ proteins on the outer layer (capsid) of rotavirus vary by rotavirus type. Image source. The existence and continued emergence of virus variants is normal for all viruses. Changes in the virus genome, called mutations, occur at random as they multiply. Mutations can have a big or small impact, and can affect the survival of the virus, its ability to adapt to new hosts, its transmissibility, disease severity and characteristics, and its ability to escape recognition by antibodies generated after previous infections or vaccination.
Rotaviruses are very diverse. They are classified into types depending on the composition of the two proteins that make up the virus’ external layer. The potential for these two proteins to appear in different combinations—through genetic exchange—increases diversity further.
The distribution of rotavirus types varies significantly between different countries and regions of the world—and within the same region from one year to the next. However, regardless of type, all rotaviruses cause the same disease, and no type has been associated with more severe symptoms.
2. Rotavirus variants have little effect on vaccine efficacy, regardless of vaccine type.
The oral rotavirus vaccines currently in use have been developed using two different general approaches. One approach relies on the vaccine containing one variant: either a weakened version of the most commonly circulating virus variant, or a variant that caused asymptomatic infection in newborn infants. This approach assumes the single variant will provide sufficient cross-protection against other rotavirus types/variants. A second approach relies on the vaccine having a combination of the most frequently found variants, with the goal of developing greater type-specific protection.
We have been studying the global diversity of rotaviruses in order to monitor whether vaccination influences the virus’ diversity. The aim is to investigate whether some rotavirus types may be found more frequently in vaccinated children, as this could indicate either that the vaccine does not protect or that it protects less well against a particular rotavirus type. We do this by comparing the diversity and types of rotaviruses found in children with diarrhea before and after rotavirus vaccination is introduced in a population. We also evaluate the diversity and types of rotaviruses causing disease in vaccinated versus non-vaccinated children in the same region of the world.
Overall, the rotavirus diversity and evolution data we have been studying for over a decade tell us that, like with natural infection, rotavirus vaccines produce a good degree of cross-protection against a variety of rotavirus types.
 Year-to-year change in distribution of the 6 most frequently found rotavirus types in 11 countries across Europe. Data source: EuroRotaNetWhile it is well documented that the efficacy of live oral rotavirus vaccines is reduced in children living in low-income countries, this reduced efficacy is unlikely to be driven by differences in rotavirus strain diversity. Some changes in the diversity of circulating rotaviruses before and after rotavirus vaccine introduction have been seen in populations in which rotavirus vaccine performance is suboptimal, as in Malawi, but similar changes have also been seen in populations where the vaccine efficacy is—and has remained—optimal, as in Europe.
Year-to-year change in distribution of the 6 most frequently found rotavirus types in 11 countries across Europe. Data source: EuroRotaNetWhile it is well documented that the efficacy of live oral rotavirus vaccines is reduced in children living in low-income countries, this reduced efficacy is unlikely to be driven by differences in rotavirus strain diversity. Some changes in the diversity of circulating rotaviruses before and after rotavirus vaccine introduction have been seen in populations in which rotavirus vaccine performance is suboptimal, as in Malawi, but similar changes have also been seen in populations where the vaccine efficacy is—and has remained—optimal, as in Europe.
3. Monitoring strain diversity before and after vaccination campaigns provides crucial information.
As a new generation of rotavirus vaccines aimed at providing better protection for the children most affected by rotavirus diarrhea is developed, monitoring their effectiveness against different rotavirus types will remain crucial. Without genetic surveillance, we cannot know what virus variants are circulating, how well interventions like vaccines are working against them, or how to change course if needed. I believe this will be crucial for COVID-19 vaccines, too.
4. Even with reduced efficacy, vaccines save lives.
Although the degree of protection against rotavirus variants closely related to the vaccine virus may be greater than that against more distantly related variants, it is important to remember that rotavirus vaccines protect children from severe diarrhea and death.
As with COVID-19 vaccines, even if the impact on infection and transmission varies by vaccine, location, and virus variant, rotavirus vaccines save many lives. Partial protection is significantly better than no protection.


