Rotavirus vaccines could be a public health game-changer in Mongolia
|

Over the past 20 years, child deaths in Mongolia have plummeted. Socioeconomic development and child health interventions are working to save lives. But of the child deaths that still occur, a main cause remains a disease that’s entirely preventable: diarrhea.
Diarrhea is a heavy burden to families and the health system in Mongolia. A 2013 survey found that moderate-to-severe diarrheal disease was affecting 8.2% of all children under five years at one time, with the highest prevalence in rural areas. Although fewer children are dying from the severe dehydration that diarrhea can bring, its wide-scale prevalence still causes undue physical, psychological, and financial suffering for Mongolian children and families.
The leading cause of severe diarrheal disease, rotavirus, is vaccine-preventable. Nearly 100 countries worldwide are already using rotavirus vaccines in their national immunization programs, but Mongolia, along with many other countries in Asia, have yet to do so. We are hopeful that will change.
Mongolia transitioned out of support from Gavi, the Vaccine Alliance in 2016, so any new vaccines must now be self-financed, without access to Gavi financing. Because Mongolia still has limited resources, it is crucial for the Ministry of Health (MOH) to critically evaluate the potential benefits, cost-effectiveness, and budget implications of new vaccine programs. Additionally, Mongolia’s National Program on Infectious Diseases Prevention and Control prioritizes the use of country-specific evidence to inform decision-making around new vaccine introduction.
A few years ago, pneumococcal conjugate vaccine and rotavirus vaccine were both in the Mongolian national immunization program (NIP)’s agenda to be considered for introduction. Following an informative cost-effectiveness analysis of pneumococcal conjugate vaccine, the country team decided to do the same for rotavirus vaccine. With the assistance of the World Health Organization (WHO) Western Pacific regional office, we became connected with PATH. Our team kindly accepted their help in conducting the analysis.
Working closely with the MOH, PATH, the WHO Mongolia country office, the Mongolian National University of Medical Science, and international experts, we gathered all of the health and costing data needed to inform the analysis. What we found was very encouraging.
We estimate that, between 2019 and 2028, a rotavirus vaccination program in Mongolia could prevent more than 62,000 non-severe rotavirus cases, approximately 34,000 severe cases, and 271 deaths. This corresponds to approximately 19,000 healthy years of life – called disability-adjusted life-years or DALYs – saved. The vaccination program could also save 44,900 outpatient visits and more than 27,000 hospitalizations and millions of dollars of health care costs. The rest of the estimates are available in our study, which was recently published in Vaccine.
A surprising finding came from the comparison of different rotavirus vaccines –ROTARIX, RotaTeq, and an India-made vaccine called ROTAVAC that was recently WHO-prequalified in 2018. While the use of any of the vaccines would be highly cost-effective, ROTAVAC resulted in a net cost approximately 70% lower than ROTARIX or RotaTeq. Accounting for the savings in health care costs, a vaccination program with ROTAVAC would be not only greatly beneficial for children’s health, but also very affordable for Mongolia.
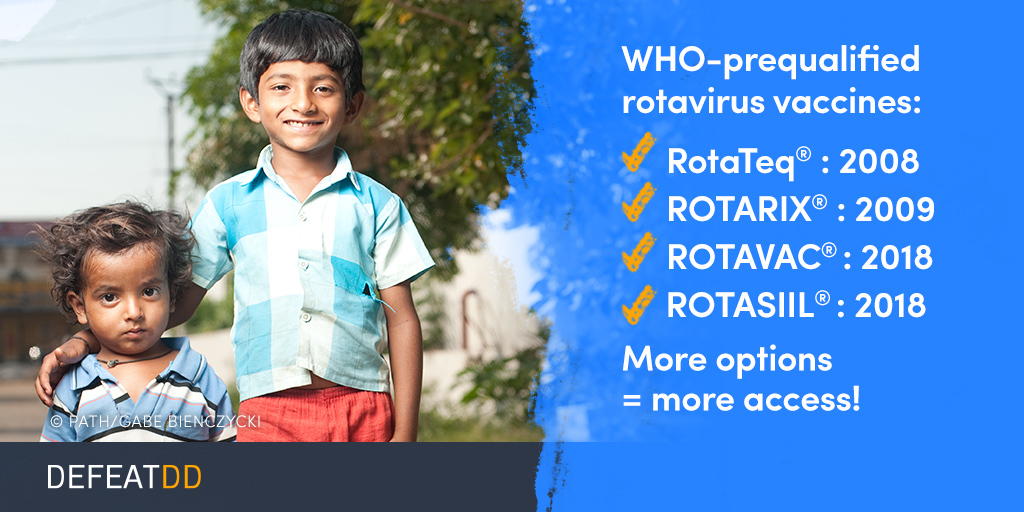
Rotavirus vaccines are a clear choice for public health and development in Mongolia. They would have both economic and health benefits to prevent severe rotavirus diarrhea, especially for the more heavily affected rural families. And based on our analysis, for Mongolia and other countries that cannot access Gavi’s finance mechanisms, any of the three rotavirus vaccines we analyzed would be highly cost-effective—especially the low-cost ROTAVAC vaccine from India.
In addition to the analysis, we also gained other benefits from the collaboration with PATH. The country team not only built local capacity on vaccine cost-effectiveness analysis methodology, but also benefitted from great opportunities to exchange experiences and learn from other countries.
As Mongolia and other regional countries continue to weigh the lifesaving decision to introduce rotavirus vaccine, we hope our analysis will prove useful.