How cost-effectiveness analysis helped strengthen Bangladesh’s resolve to combat rotavirus
|

In the lead-up to Bangladesh’s introduction of rotavirus vaccines, a recently published cost-effectiveness analysis helps bolster the evidence base for decision-makers.
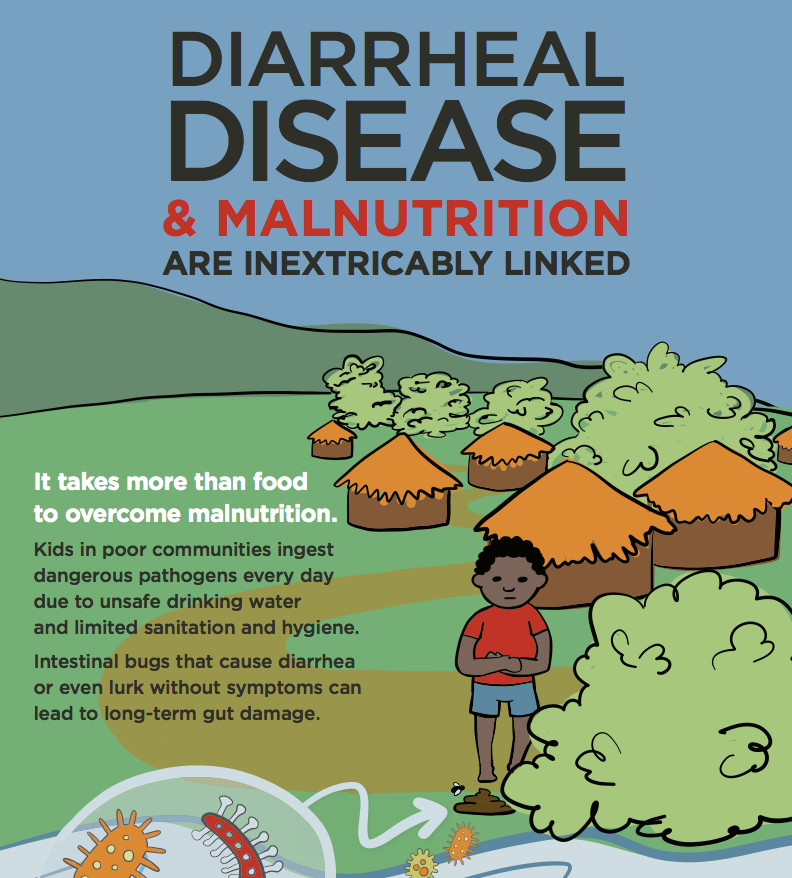
Bangladesh has long played a leading role in building the evidence base for interventions to combat diarrheal disease. This includes early groundbreaking research on oral rehydration solution as well as a pivotal RotaTeq® rotavirus vaccine effectiveness trial that contributed to the 2009 World Health Organization (WHO) recommendation for global rotavirus vaccination. Researchers in Bangladesh also recently completed an effectiveness trial of Rotarix® in Bangladesh to round out the evidence. So it is no surprise that Bangladesh is once again taking a leading role in its upcoming introduction of rotavirus vaccines.
Bangladesh was approved for Gavi support of rotavirus vaccination in 2016 and plans to introduce the vaccine in its national immunization program in 2018. This will be among the first Gavi-supported national introductions of rotavirus vaccines in Asia. After Bangladesh made the decision to introduce, the government and its partners wanted additional information about potential health impacts and cost-effectiveness of the vaccine. To help support the country’s decision and inform implementation efforts, the Bangladeshi immunization program worked with PATH, CDC, the Liverpool School of Tropical Medicine, WHO, and the London School of Hygiene & Tropical Medicine to generate this evidence through a cost-effectiveness analysis.
The analysis, which was recently published in Vaccine, used the Pan American Health Organization’s TRIVAC model, which is designed for countries to conduct vaccine cost-effectiveness analyses by inputting data into an Excel-based model. I was brought in to contribute knowledge on topics such as disease burden and to provide perspective based on my experience with similar studies around the world. With inputs and expertise from the Bangladeshi immunization program and several partners, the model estimated that rotavirus vaccination would be considered cost-effective or highly cost-effective for Bangladesh in all possible scenarios considered—with or without a Gavi subsidy, and even with low mortality. The model also generated estimates the vaccination program costs to inform country budgeting. Armed with this evidence, the immunization program can now feel even more confident in its decision to introduce rotavirus vaccines.
Cost-effectiveness analysis is a very useful tool, this evidence has served and continues to serve an important role for decision-makers and partners in Bangladesh. The results of the analysis will help build and sustain support for the country’s introduction of rotavirus vaccines in 2018, which will have an incredible impact on children’s lives and health, on families’ wellbeing, and on the capacity of the health system. It may also help build support for rotavirus vaccination in the rest of the region, as other countries in Asia can look to this analysis for insight on their own immunization programs. The results of the analysis will be especially useful for Asian countries that may not be Gavi-eligible or that may have lower rotavirus mortality rates.
I am so excited to see Asian countries finally adopting rotavirus vaccines—and so grateful to Bangladesh for leading the way.
Disclaimer: The opinions expressed are those of the author and do not reflect the official position of the US Centers for Disease Control and Prevention.
Photo credit: PATH.