How does human milk banking help ensure child health?
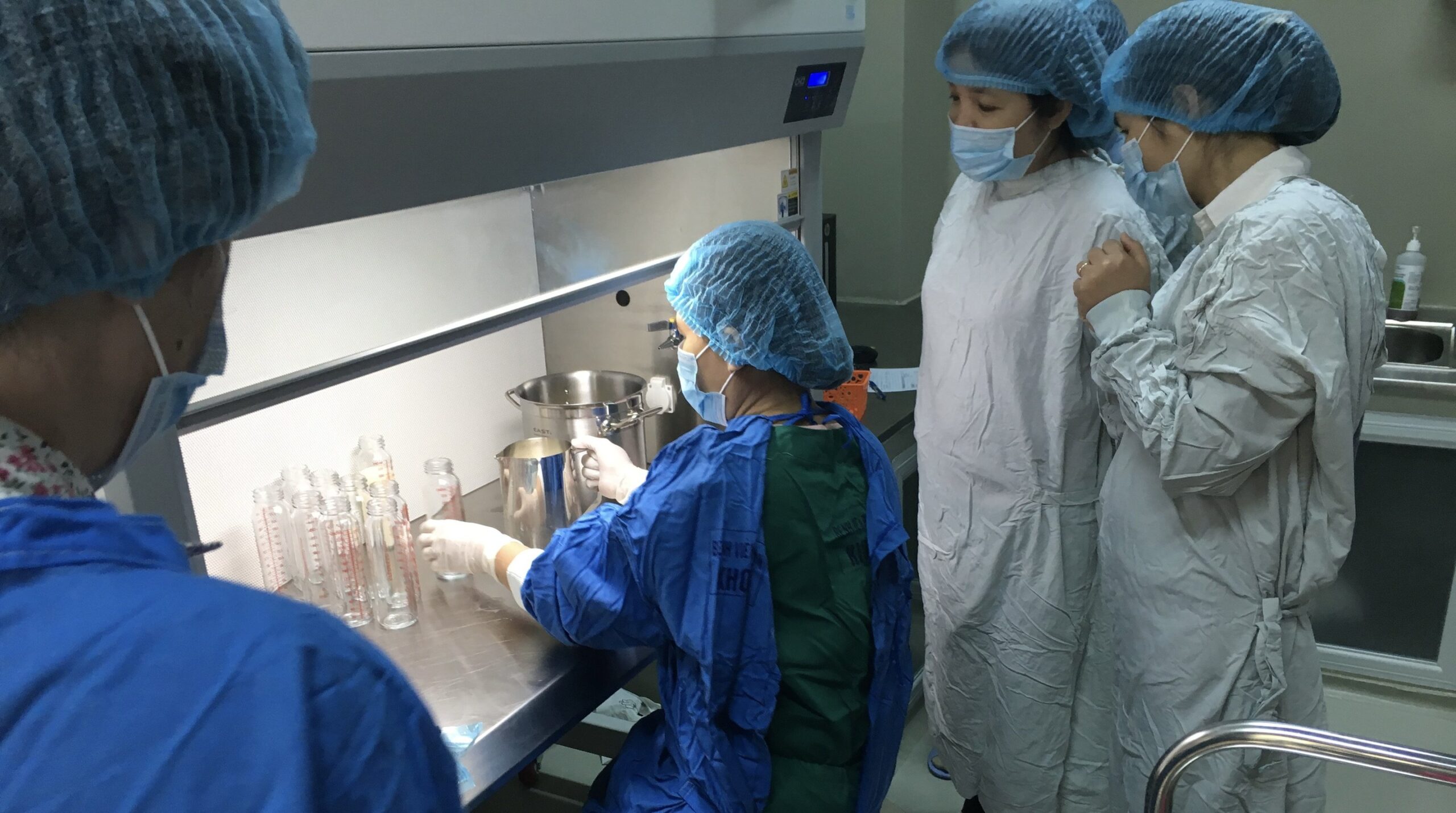
At a human milk bank in Vietnam, health workers divide donated milk into bottles for newborns. Photo: PATH.
This article was originally posted on PATH.org, the link can be found here.
When a mother is unable to breastfeed, donor milk can make all the difference, especially for small, preterm, and sick infants.
The World Health Organization recommends breastfeeding for infants to support healthy growth and development. But why is this recommended? And when women face barriers breastfeeding, what alternatives exist to provide nutrients to newborns?
To answer these questions, let’s learn more about the nutritional value of breastmilk and the benefits of donor milk from human milk banking.
Why is breast milk important to child health?
Superior to formula, human milk provides essential nutrients for infant growth and development. According to UNICEF, “feeding infants nothing but breastmilk guarantees them a food source that is uniquely adapted to their nutrient needs, while also being safe, clean, and healthy.” Despite the nutritional benefits of human milk, less than half of infants under six months old are exclusively breastfed.
Infant mortality remains high globally as millions of babies die within their first year of life. Unfortunately, numerous social, political, and structural barriers can hinder a mother’s ability to breastfeed. These often include the influence of social norms, lack of support for breastfeeding mothers, and impact of infant formula marketing. Additionally, women may lack knowledge about the benefits of breastfeeding or are simply unable to produce enough breastmilk. To help address some of these barriers, PATH is working collaboratively with governments and partners worldwide to increase equitable access to human milk.
What is human milk banking?
Human milk banks play an essential role in newborn health by providing human donor milk to newborns who would otherwise not be able to receive their mothers’ own milk. This is necessary for newborns that are small and/or sick, meaning those that are born preterm, are small for their gestational age, have low birth weight, have an illness or birth complication, as well as those requiring hospitalization. Donor human milk is specifically targeted to this population of newborns.
Donor human milk is used as a bridge, while the mother’s lactation supply can be established and the infant transitions to feeding directly from the breast, equipping both mother and baby for healthy breastfeeding post-discharge. Milk banks collect, screen, store, process, and distribute human milk. Women who donate milk usually breastfeed their own infants and have a milk supply that exceeds their own infants’ needs. Best practice is to implement human milk banks as a component within a comprehensive and integrated system, to ensure they are in line with the broader purpose of protecting, promoting and supporting breastfeeding and child nutrition.
Human milk banks are increasing worldwide, as the global health community recognizes the benefits of such efforts on newborn health. PATH works at a global level advocating for exclusive human milk diets and with Ministries of Health to ensure a sustainable and locally appropriate human milk bank system is embedded within newborn care and breastfeeding promotion—such as our work in Kenya. Furthermore, PATH has resources available for establishing and integrating human milk banks into existing health facilities to expand global access. PATH toolkits detail how to ensure appropriate use of donor human milk and how to introduce a rigorous human milk bank system for screening, pasteurizing, storage and distribution, all of which is required to ensure safe donor human milk. These essential efforts help to provide equitable access to human milk for babies around the world.
Human milk banks help prevent diarrhea
Given what we know about the nutritional benefits of human milk, and the accessibility challenges of this feeding option for newborns, exclusive human milk diets contribute to preventing and reducing diarrheal disease. Infants are at greatest risk of diarrheal disease when they are given foods other than breast milk. This is because they are more likely to be exposed to food- and water-borne pathogens and lose the protection of breast milk’s anti-infective properties. Furthermore, diarrhea is a leading cause of malnutrition in children under five, and malnourished children are more vulnerable to infection. Human milk helps an infant’s immune system to safeguard against infectious diseases like diarrhea and other dangerous pathogens.
Breastfeeding and safe provision of donor human milk are significant in efforts to defeat diarrheal disease: we encourage stakeholders, health providers, and other advocates to strengthen systems to support exclusive human milk diets and utilize available milk banking resources, when appropriate, to advocate for expanded access to nutritional breastmilk for infants in all regions of the world.


