What Can Psychological Context Bring to Safe Water Interventions?
|

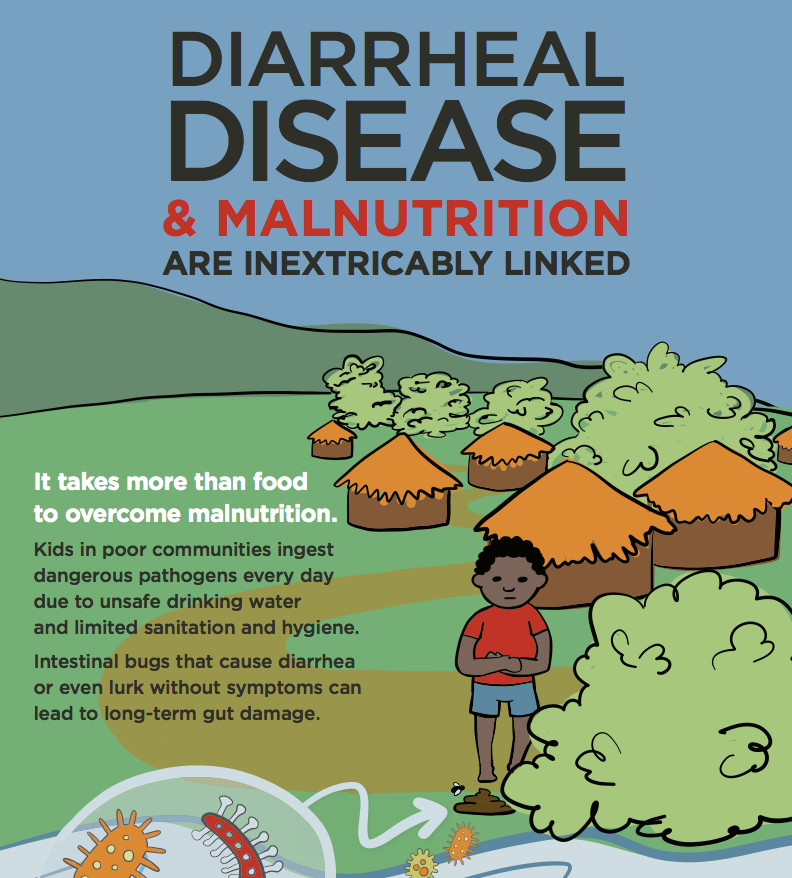
Because unsafe water supplies and sanitation account for most life-threatening diseases among children in developing countries, the provision of safe water and improved hygiene is a central focus of global health projects. And in addition to current public health research and practices, biology, and engineering, the success of these projects also relies on behavioral change at individual and cultural levels. Psychologists and anthropologists have an important role to play.
For the past three years, my former graduate student Heidi Beebe, now a visiting assistant professor of psychology at Pacific Lutheran University in Tacoma, WA, and I have been evaluating human cognition and behavior related to contamination in Sub-Saharan Africa. As developmental psychologists, we study cognition and its development in social and cultural context. We are especially interested in children's skill at detecting when water and food are safe to consume, called contamination sensitivity. We are also interested in how people learn about contamination. We largely focus on children 4- to 12-years of age because they spend much time outside of adult supervision and engage in chores involving water. Although our research is based on studies that have shown that contamination sensitivity develops from early to middle childhood, most existing research has been conducted in industrialized settings where the risk of contamination is low.
In the rural Kibaale District of western Uganda, we interviewed 48 people between 4 and 60 years of age, presenting 23 different images of water and food that was contaminated (or not). Most participants rejected contaminated items and did not reject uncontaminated items. However, performance was not perfect, and younger children showed a lack of clarity in some instances. Most participants said they would not drink water from a pond with animals nearby because germs or droppings would remain, suggesting some understanding of residual effects. Most also rejected juice with a bug in it, but some younger children said they would drink the juice if the bug was removed. We also asked how they learned their contamination knowledge. Most children said they learned about contamination from family members or teachers; adults reported learning it in school.
In a second study outside Arusha, Tanzania, we interviewed 74 children, 4 to 9 years of age, about 10 scenarios presented in a set of drawings that depicted contamination (or not). Most children rejected contaminated items, but older children were more likely to, suggesting that children under 7 years have more health risk when deciding about contamination on their own. Children reported learning this information at home, mostly from siblings, and at school.
In Maasai villages in northern Tanzania, where homes do not have running water and people wait hours or days to fill containers at local sources, we interviewed 40 adolescents and 23 adults about their knowledge of stomach illness, germs, and water contamination. Adolescents had more biological knowledge, knew more about germs and preventing stomach illness, and relied more on Western treatments and medicines than adults. They reported learning this knowledge at school and passing it onto children and adults at home.
Overall, our studies yielded some interesting insights:
-- Children's knowledge of contamination in Sub-Saharan Africa is in some aspects more advanced than has been found among children living in industrialized regions.
-- Younger children may over-correct and avoid uncontaminated substances, which suggests limited understanding.
-- Germ knowledge and causal reasoning about stomach illness is greater among adolescents than adults in rural areas.
-- Adolescents are more receptive to Western medicine and innovative decontamination methods than adults.
-- Adults may be receptive to learning health information from youth.
This information can be useful to health workers as they try to improve water-related practices and sanitation in the developing world. Successful program interventions will rely on bridging clinical and psychological contexts to provide clinical prevention and treatment that are developmentally appropriate and respect local understanding and practices.
Photo credit: PATH/Gareth Bentley.