A promising new tool to identify children at highest risk of long-term health issues caused by diarrhea
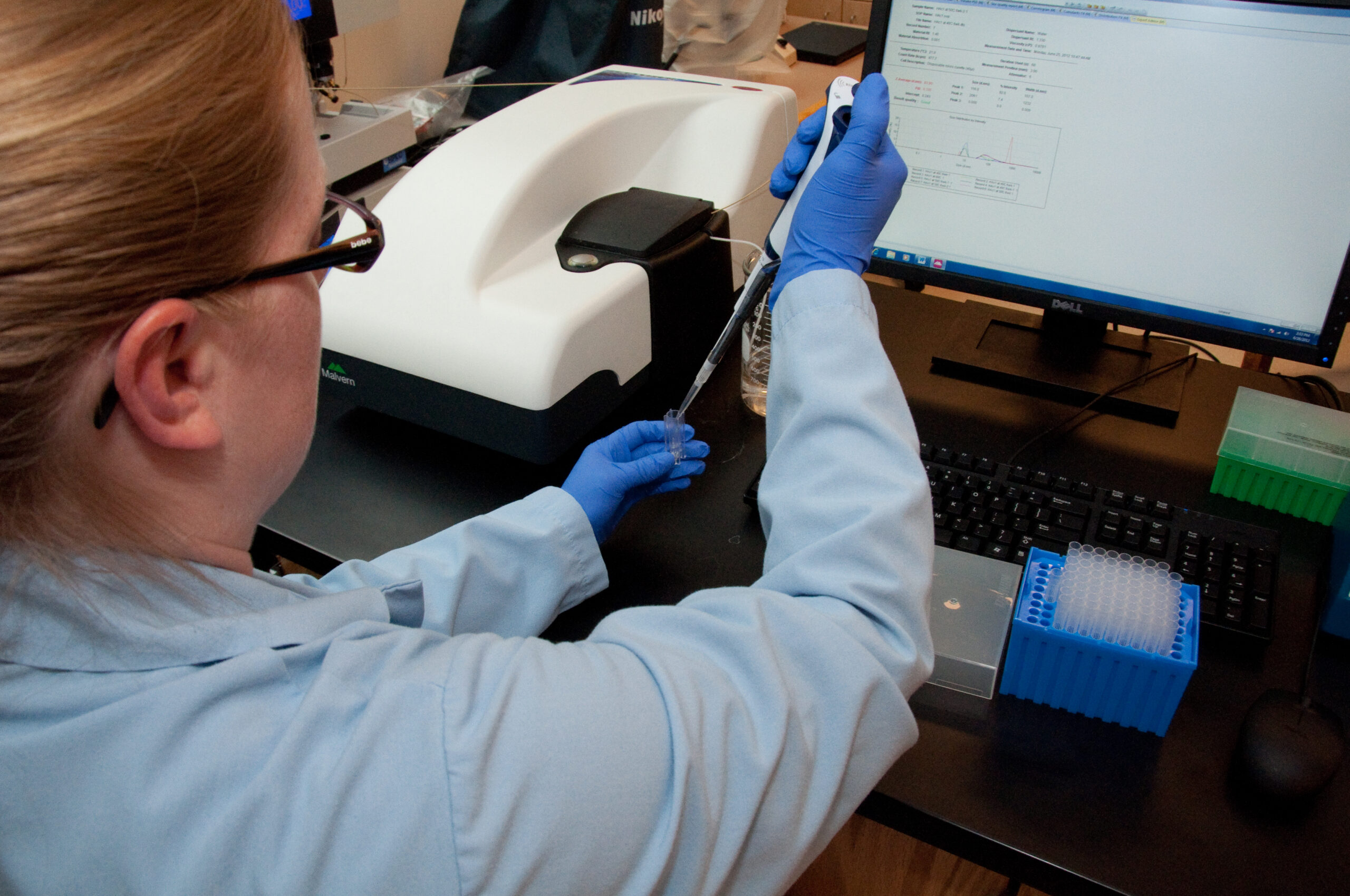
A new laboratory diagnostic tool can help identify environmental enteric dysfunction (EED) in children using biomarkers related to micronutrients, growth, inflammation, and oral vaccine immunogenicity. Photo: PATH
We all know that children experiencing diarrhea are suffering. But what happens to children’s bodies after an acute diarrhea episode? Particularly children who experience multiple diarrhea-causing infections each year and who may also be malnourished? Environmental enteric dysfunction (EED) is an intestinal disorder common among children in low-resource settings and is associated with an increased risk of growth stunting, cognitive deficits, and reduced oral vaccine efficacy. The combination of malnutrition and persistent gut infections (e.g., viruses, bacteria, and parasites that cause diarrhea) in early childhood may cause the structural gut damage and impaired intestinal function indicative of EED. This can lead to lifelong negative impacts on children’s health and well-being.
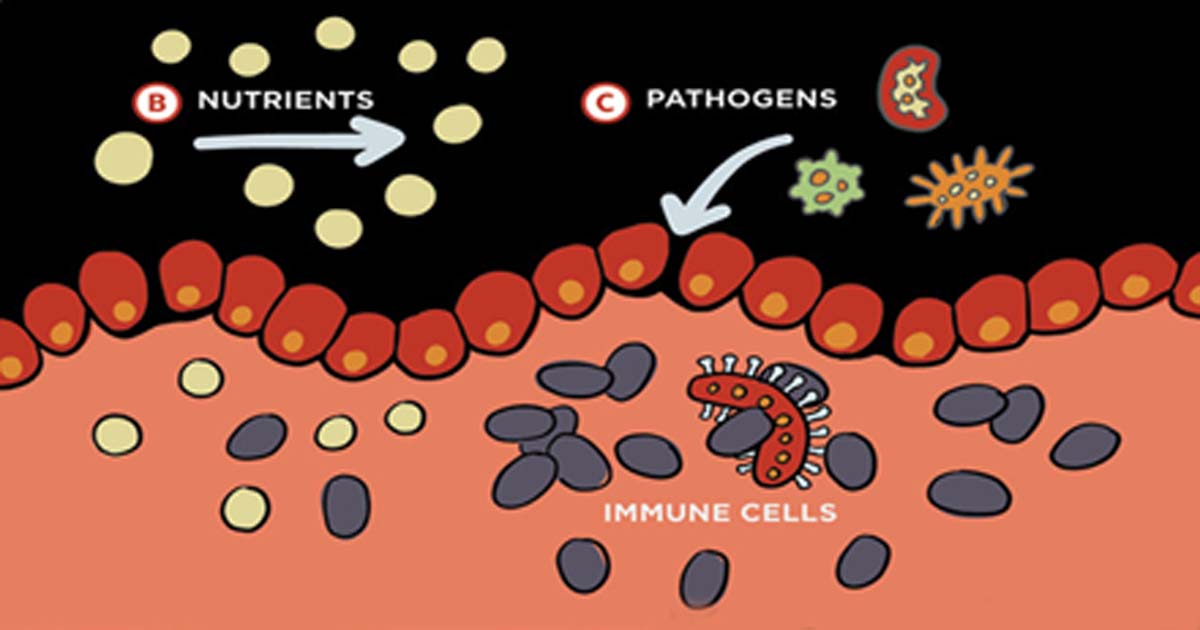 Environmental enteric dysfunction (EED) resulting from diarrheal infections can cause damaged gut lining and long-term effects such as malnutrition and stunting.A key challenge to identifying children with EED at highest risk of these long-term health concerns is the lack of validated predictive biomarkers (early warning systems for your health). Ongoing clinical studies are testing and validating EED biomarkers in child populations at risk for stunting, yet testing multiple biomarkers commonly requires specialized equipment, complex methods, resources, and considerable effort.
Environmental enteric dysfunction (EED) resulting from diarrheal infections can cause damaged gut lining and long-term effects such as malnutrition and stunting.A key challenge to identifying children with EED at highest risk of these long-term health concerns is the lack of validated predictive biomarkers (early warning systems for your health). Ongoing clinical studies are testing and validating EED biomarkers in child populations at risk for stunting, yet testing multiple biomarkers commonly requires specialized equipment, complex methods, resources, and considerable effort.
To meet the need for an effective, affordable research tool that enables the measurement of multiple EED biomarkers and micronutrients from children in low-resource settings, PATH has co-developed the Micronutrient and EED Assessment Tool (MEEDAT). The MEEDAT aims to measure biomarkers associated with child growth faltering and oral vaccine immunogenicity, as well as biomarkers indicative of systemic inflammation and micronutrient deficiencies. PATH and partners conducted a study to validate the MEEDAT using 300 samples from infant clinical trial participants in Mali to evaluate biomarker risk factors for growth faltering and vaccine failure, the results of which were published recently in PLOS Neglected Tropical Diseases.
To learn more about the study and what the results could mean for children’s health, we talked with the lead study author, Dr. Michael Arndt. Mike helped develop the MEEDAT as a post-doctoral fellow at PATH, and he’s now a Research Scientist at the University of Washington’s Institute for Health Metrics and Evaluation in Seattle.
DefeatDD: How did the MEEDAT perform in this study?
Mike: MEEDAT performed quite well in comparison to commercially available enzyme-linked immunosorbent assays (ELISAs) that measure the four biomarkers that were added to the existing 7-plex multi-micronutrient assessment tool: soluble CD14 (sCD14), intestinal fatty acid binding protein (IFABP), insulin-like growth factor 1 (IGF-1), and fibroblast growth factor 21 (FGF21). The correlation between the output from MEEDAT and each of these ELISAs ranged from 0.8 to 0.97, indicating that their results were very similar, which is fantastic! Furthermore, we were able to observe several associations between the markers measured and oral vaccine immune response and growth.
DefeatDD: Why was it important to conduct this study?
Mike: It was essential to demonstrate the performance of the MEEDAT in comparison to standard methods for measurement of blood-based biomarkers so that scientists in this field could be confident that the output from MEEDAT is adequately measuring the same markers as existing methods (e.g., ELISA) that have been used in past pediatric clinical and observational studies. Another key point was demonstrating the efficiency of MEEDAT; from as little as 10 to 20 microliters of serum, researchers can obtain values for 11 different biomarkers. This is in contrast to standard ELISAs that often require five times more serum, but only provide data for a single biomarker.
 MEEDAT utilizes an assay well plate to test various biomarkers related to EED.DefeatDD: How can the MEEDAT help improve children’s health?
MEEDAT utilizes an assay well plate to test various biomarkers related to EED.DefeatDD: How can the MEEDAT help improve children’s health?
Mike: MEEDAT will offer a rapid and effective tool for efficiently screening children for EED prior to enrollment into clinical trials of candidate EED interventions. Using MEEDAT will also streamline the evaluation of efficacy in trials for which the biomarkers are included as clinical endpoints. MEEDAT can reduce the time and cost involved and increase the accuracy of plasma-based biomarker measurement among children at risk for or already suffering from malnutrition in clinical research and accelerate the identification and deployment of effective interventions.
DefeatDD: What’s next for the MEEDAT?
Mike: MEEDAT will be used in several planned studies with samples collected from children in low-resource settings to further explore the relationship between levels of these biomarkers, EED, and growth stunting. In addition, MEEDAT is being commercialized by Quansys Biosciences in partnership with PATH and will be available by the end of 2020. PATH is working with several partner institutions to test samples they’ve collected, or will soon collect, from various EED studies in low-resource settings. PATH is also interested in developing a MEEDAT version 2.0 that would add other biomarkers onto the panel in order to increase the sophistication of the types of analyses we could perform with it. Lastly, PATH is planning a new companion tool for MEEDAT, dubbed the Fecal EED Assessment Tool (FEAT) that would measure EED biomarkers in fecal samples, which in some cases are easier to collect than blood samples.


