The true cost of vaccine-preventable diarrhea in Africa
|

Vaccines against diarrheal disease still have an enormous amount of untapped potential for Africa—for children’s lives, their ability to flourish, their families’ livelihoods, and their countries’ economies.
The Ministerial Conference on Immunization in Africa is currently underway. Leaders from across the continent have gathered in Addis Ababa, Ethiopia, to discuss how to achieve universal immunization coverage in all African countries and, in doing so, avert vaccine-preventable deaths and disabling diseases from limiting the potential of African children.
To help country decision-makers determine the best use of limited resources, Atherly’s team at PATH evaluates the costs and public health impacts of vaccines.
As with all public health decisions, the cost of immunization programs is an important consideration. Public officials have an important responsibility to spend public funds in a way that benefits the highest number of people. We already know that vaccines in general are one of the best buysin global health, and vaccines against diarrheal disease, which is responsible for 12 percent of deaths of African children under five years old, are no exception.
The financial burden of diarrhea
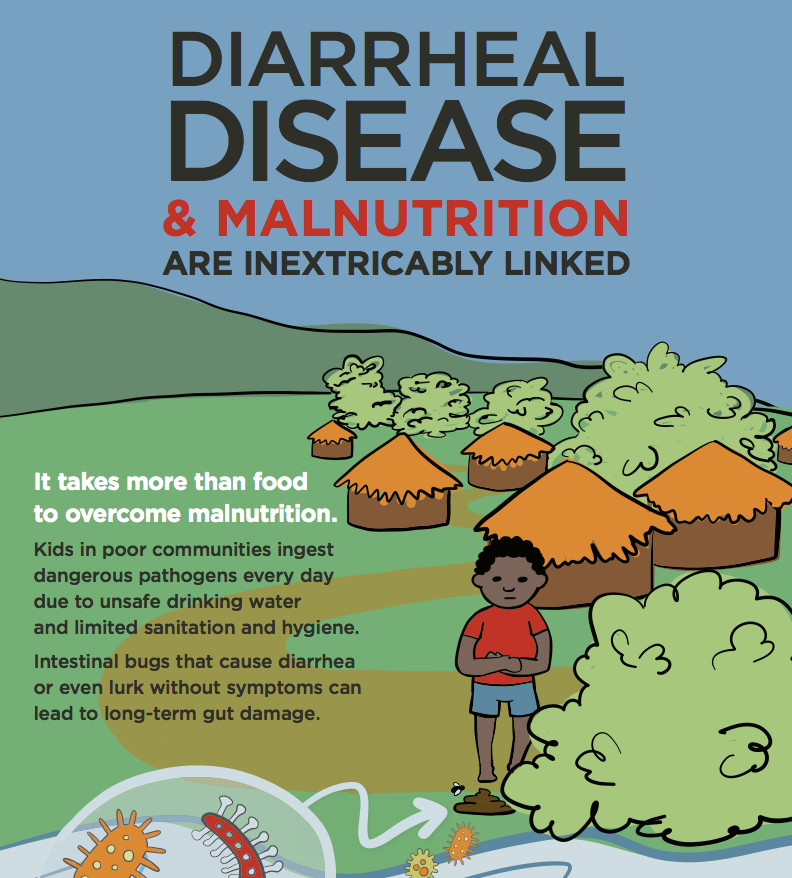
Diarrhea imposes a large public health burden—not just in terms of death and illness, but also in terms of finances. When a young child in a developing country gets sick with diarrhea, his or her parents usually have to pay for the care, which can amount to a significant portion of the family’s income. Additionally, because the parents have to stay home and take care of their child, or take him or her to a hospital, they lose wages that they would have otherwise made at their jobs. And then—on top of all that—often when one child gets sick, the infection is passed on to other children in the family. Having multiple sick children in the same household can be financially devastating for a family.
But what we also have to understand about diarrhea is that, when a child has multiple episodes of diarrhea, he or she is left more vulnerable to other infections, malnutrition, and stunting, which can have a lifelong toll on that child’s ability to grow, thrive, and contribute to society.
That is why we have to prioritize vaccines against diarrheal disease.
The promise of vaccines
Vaccines against rotavirus, the leading cause of severe and deadly diarrhea among children under five years of age, have now been introduced in 33 countries in Africa—27 of which are Gavi-eligible—and have a wealth of evidence on both their projected and real-world impact.
In 2012, I published an article on the projected health and economic impact of rotavirus vaccines in 72 countries eligible for support from Gavi, the Vaccine Alliance. Our model told us that, indeed, rotavirus vaccination would be considered very cost-effective in all of these Gavi-eligible countries—especially those in Africa, the region with the highest burden of diarrheal disease. Four years later, we are starting to see our projections come to life. In Rwanda, a recent study just revealed a 50 percent decline of all-cause childhood diarrheal hospitalizations following the introduction of rotavirus vaccines. And in Malawi, hospital admissions for diarrhea declined by 43 percent after the rotavirus vaccine rollout.
Additionally, vaccines against two of the other leading causes of severe diarrhea—enterotoxigenic E. coli (ETEC) and Shigella bacteria—are currently under development. While a lot more research will be needed before they can be introduced in countries, early estimates indicate the vaccines would be highly cost-effective in low-resource settings. We hope this evidence will help decision-makers as they consider and potentially plan for ETEC and Shigella vaccine introduction in years to come.
Saving lives, saving costs
We cannot afford to let any more children miss out on the protection of lifesaving, life-improving, and highly cost-effective vaccines against diarrheal disease. Diarrhea caused by rotavirus alone costs the lives, livelihoods, hopes, dreams, and futures of hundreds of thousands of children across Africa every year. For their families, the impact of rotavirus vaccination programs means more than just economics.
As countries with rotavirus vaccination programs have already shown, it means that more children can live past their fifth birthday. It means more children who are able to live to the full extent of their potential, not held back by disability, stunting, long-term illness and expensive hospital visits, or early death caused by rotavirus diarrhea. It means more parents are better able to take care of their children, work productively, and contribute to growing economies.
The cost of not introducing vaccines against diarrheal disease is just too high. By prioritizing vaccines against diarrheal disease, leaders across Africa can help ensure that African children and their families not only survive, but thrive—both physically and financially.
Photo credit: PATH/Gabe Bienczycki.