Electing cost-effective vaccines
|

This post originally appeared on Vaccineswork.org.
This year’s US election was unforgettable for many reasons. It was particularly memorable for me because, as the final results were coming in and most Americans were asleep, I was sitting in the middle of a workshop in Bangkok, Thailand. I was among participants from Nepal, Bangladesh, Afghanistan, Myanmar, Bhutan, and several global health agencies and partners who had gathered for a three-day workshop co-hosted by PATH and the International Vaccine Access Center at Johns Hopkins University on how to use health economics evaluations to inform rotavirus vaccine introduction decisions. While the Americans in the group were trying our best to focus on the afternoon’s agenda and not be distracted by the election results, our resolve eroded when we saw that all of the participants were doing the same. The collective decision of US voters was a global affair with potential implications for all countries around the world.
This experience not only reinforced just how interconnected our world is; in a way, the concurrence of the election and the workshop also provided a reminder of the importance of evidence-based decision-making. Just like voters, country leaders and decision-makers must “elect” policies, programs, and interventions based on the evidence that they have in front of them. In case of the US election, competing claims and conflicting information made the “evidence” for each candidate murky for many voters. Fortunately, in the case of rotavirus vaccine introduction, the evidence is much clearer.
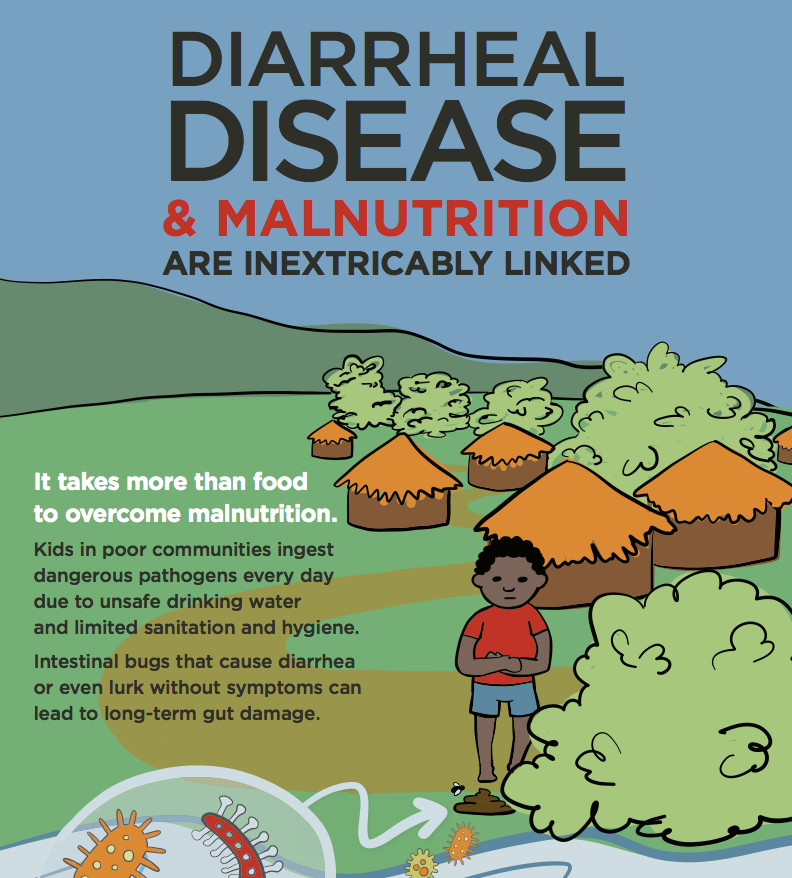
Rotavirus vaccines not only improve child health but also save lives. Vaccination lessens the tremendous economic and health burden of rotavirus disease, contributing to poverty reduction and improved economic outcomes. Published cost-effectiveness analyses have consistently concluded that the introduction of rotavirus vaccines into low- and middle-income countries would be cost-effective or, in many cases, highly cost-effective.
Such analyses have historically been conducted by global health agencies and donor-funded projects, usually targeting high-burden priority countries. New cost-effectiveness analysis methods and tools, however, such as the updated and enhanced UNIVAC model from the ProVac Initiative and the London School of Hygiene and Tropical Medicine, are making it possible for trained country EPI staff and partners to lead economic analyses of vaccine introductions in their own countries. With high-quality evidence specific to their own country, decision-makers can feel confident in choosing to invest in rotavirus vaccines and shape their programs in the most cost-effective manner.

This is why we held the workshop—to equip these decision-makers with these new methods and tools as well as provide an overview of how to interpret, disseminate, and use cost-effectiveness analyses to make decisions about rotavirus vaccine introduction. For middle-income countries and those graduating from the support of Gavi, the Vaccine Alliance, such tools can prove invaluable in the process of deciding how to spend limited government resources in the way that will most benefit their country’s health and economy. After the workshop, participants expressed increased confidence in presenting the evidence for new vaccine introduction to key decision-makers in their country, and PATH and partners are offering follow-on support to help participants undertake their own rotavirus vaccination cost-effectiveness analyses. A second rotavirus health economics workshop is planned for the Eastern European region in 2017.
Decisions—whether it is an individual voter’s decision in an election, or a leader’s decision to introduce a new public health intervention like rotavirus vaccines—are ideally based on careful consideration of available evidence. Cost-effectiveness analyses are a powerful type of evidence, and we believe all decision-makers should not only have access to them, but understand how to use them as well. Just like the global implications of an individual country’s election, the decision of one country to introduce a lifesaving vaccine can have cascading benefits for communities, regions, the world, and generations to come.
Photo credits:
GAVI, Evelyn Hockstein
PATH, Devin Groman